How do we keep updated????
Polycystic Ovarian Syndrome (PCOS)
Polycystic Ovarian Morphology (PCOM)
I attended a professional development workshop recently, which reinforced how much I love our profession. Sonography is such a diverse, ever changing expansive profession.
“But also realised how much I still don’t know or have to learn”.

Written by : Gail Crawford (Director IUE/ Tutor Sonographer)
I’ve been scanning now for over 15 years now….but the landscape is just constantly changing; there is so much to know about each facet of ultrasound; Obstetrics, Gynaecology, Musculoskeletal etc. Not only do we need to know in detail human anatomy, but then the pathology associated with these regions. We need to keep up to date with machine technologies and how to use them, along with following the recommendations from our peers and professional bodies; understanding the current trends, techniques; topical research and criteria in diagnosing these pathologies…
Sometimes I feel like I am swamped trying to keep up…………
So what did I learn from this recent workshop??
My take home message, is that as sonographer’s we need to keep abreast with the most up to date recommendations, and ensure that we “share” these with our colleagues; ensuring we are all practising using the same guidelines, and don’t get overwhelmed by how quickly our profession is changing.
A lot of written texts are being quickly superseded by online resources, which can be updated regularly.
In regards to Obstetrics and Gynaecology reviewing the recommendations from National and World experts online; is a great start.
Entities such as:
One subject that was brought to my attention recently was:
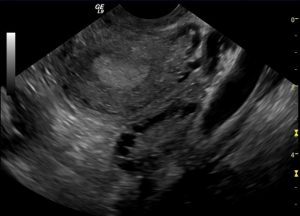
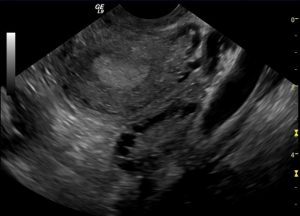
Polycystic Ovaries (PCO) – what are the Ultrasound features of the condition ????
To be diagnosed with Polycystic Ovarian Syndrome (PCOS), both clinical and biochemical (hyperandrogenism) criteria need to also be evaluated.
A lot of written text, and old online references state the following (based on the Rotterdam Criteria) for diagnosis on ultrasound of PCO:
- Enlarged ovaries (Bilateral) >10 mL
- > 12 peripheral immature follicles (string of pearl appearance)
- Hyperechoic central stroma.
This has been “superseded” by the current criteria as of 2018, put together at by Specialised Obstetric and Gynaecological Imaging Australia.
The document is titled:
“International evidence-based guideline for the assessment and management of polycystic ovary syndrome 2018”.
Criteria for PCOM:
In summary;
- Transvaginal imaging of the ovary is thought to be best method of evaluating the ovary, in sexually active patients.
- > 20 small immature follicles (Can be unilateral), in the absence of a corpus luteum or dominant follicle
- Immature follicles are less than 9mm in size (Generally 2-9mm)
- Enlarged ovary ≥10 mL
- Hyperechoic central stroma +/-
Reporting recommendations have also been made to ensure Standardisation of Written Ultrasound Reports for patients with PCOM:
Happy pelvic and gynaecological scanning😊
Please feel free to offer me feedback or discuss such topics.
References:
- Revised 2018 “International evidence-based guideline for the assessment and management of polycystic ovary syndrome”, Monash University, Melbourne Australia https://www.monash.edu/__data/assets/pdf_file/0004/1412644/PCOS_Evidence-Based-Guidelines_20181009.pdf
- Revised 2003 “Consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome”. Fertil. Steril. 2004;81 (1): 19-25)
- Wang R & Willem J (2017) The Rotterdam criteria for polycystic ovary syndrome: evidence-based criteria? Human Reproduction, Volume 32, Issue 2, 1 February 2017, Pages 261–264, https://academic.oup.com/humrep/article/32/2/261/2452298